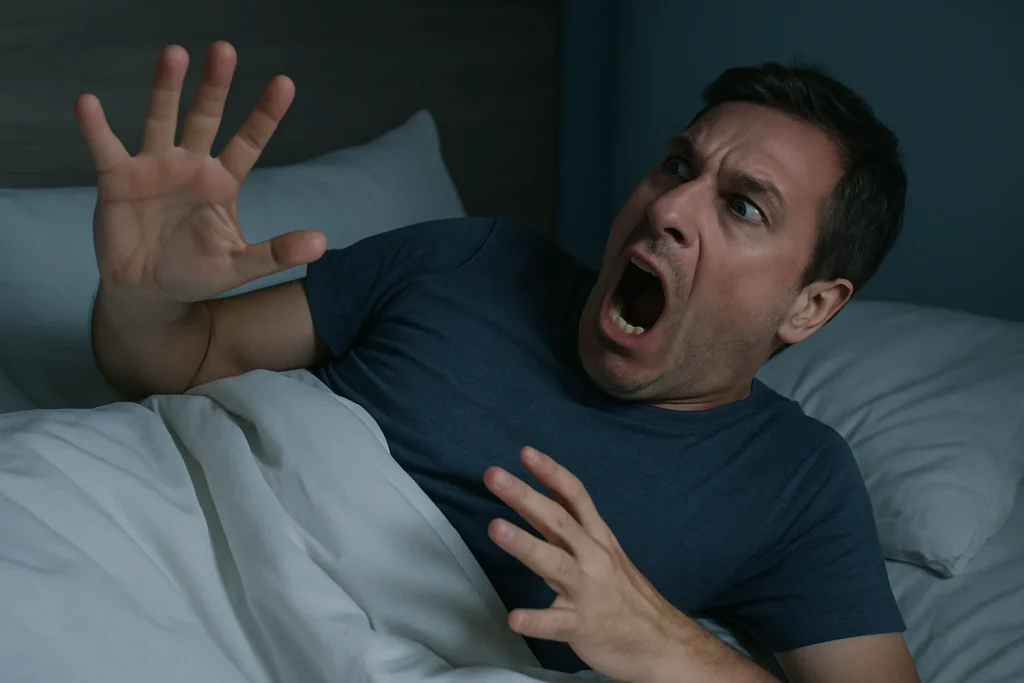
Sleep is a time when the body should rest, recover, and recharge. But for individuals experiencing REM sleep behavior disorder, nighttime becomes unpredictably active and even dangerous. Instead of the temporary paralysis that normally occurs during rapid eye movement (REM) sleep, those with this condition physically act out their dreams—sometimes violently—without any awareness of what’s happening.
At 8 Hours Sleep Clinic, we understand how disruptive and frightening these nighttime behaviors can be—not just for the patient, but for partners and family members as well. Recognizing this disorder early and seeking professional evaluation can significantly improve safety, sleep quality, and long-term health outcomes.
In this in-depth guide, we break down why REM sleep behavior disorder occurs, how it differs from other nighttime conditions, the red flags you should never ignore, and the treatment strategies that bring relief and restore a sense of security at night.
Understanding What Makes REM Sleep Behavior Disorder Unique
During healthy REM sleep, the brain is active, and vivid dreams occur while the body remains physically still. But in individuals with REM behavior disruption, the neurological “switch” that paralyzes the muscles doesn’t activate properly. This allows dream-related movements to become physically real.
Patients with the disorder may display mild or intense behaviors, ranging from small twitches to full-body movements. It is one of the few sleep conditions in which the sleeper’s actions directly mirror the content of their dreams.
What makes this disorder particularly concerning is its association with neurological health. Many sleep specialists consider it one of the earliest indicators of potential neurodegenerative changes later in life. That’s why early recognition and evaluation are essential.
Common Indicators: What RBD Looks Like at Night
Understanding RBD symptoms helps individuals and families recognize when seemingly random nighttime movements are signaling something more serious. People with this disorder may:
- Shout, talk, scream, or respond vocally to dream content
- Punch, kick, jerk, or thrash during sleep
- Fall out of bed due to intense dream reenactments
- Show sudden limb movements that align with dream scenarios
- Exhibit repetitive actions during specific moments of the REM cycle
- Wake up confused about injuries or bruises
Unlike sleepwalking, which occurs during non-REM stages, this condition is tightly linked to active dreaming. Patients often remember the dream vividly, but not the movement.
Why Acting Out Dreams Happens
One of the most recognizable characteristics of the disorder is acting out dreams at night, which can be startling and potentially dangerous. These dream-based actions happen because the brain does not properly suppress muscle movement.
In a typical night, REM sleep cycles occur every 90 minutes. During these phases, the brain sends signals that immobilize the body. But when the neural circuits responsible for this “muscle silence” become impaired, the dream content is physically expressed.
Triggers and contributing factors may include:
- Chronic stress or significant emotional strain
- Neurological disorders
- Certain medications, especially those affecting brain chemistry
- Withdrawal from specific substances
- Sleep deprivation
- Genetic predispositions
It’s critical to recognize these behaviors not as normal movement during sleep, but as indicators of a potentially serious neurological issue.
How RBD Fits Into the Spectrum of Parasomnias
While it may seem similar to sleepwalking, night terrors, or confusional awakenings, this disorder is classified under parasomnia disorders, which include conditions where unusual behaviors occur during sleep. However, REM behavior disorder is unique because:
- It occurs specifically during REM sleep
- Movements directly correlate with the sleeper’s dream content
- It tends to become more pronounced with age
- Physical injury to self or partner is more common
- It may be an early neurologic marker rather than a temporary disruption
This connection to deeper neurological pathways makes it one of the most clinically significant parasomnias.
RBD as Part of a Larger Sleep Disorder Framework
Some individuals with REM behavior disruption also experience other nighttime abnormalities that fall under sleep movement disorders. These conditions share traits such as involuntary muscle activity, disrupted rest, and altered sleep cycles.
Examples include:
- Periodic limb movement disorder (PLMD)
- Restless legs syndrome (RLS)
- Sleep-related rhythmic movement conditions
- Nocturnal muscle spasms
Because these disorders can interact, accurate evaluation is essential for developing a precise treatment plan.
The Importance of Professional Testing: How Specialists Confirm RBD
Early evaluation is essential to protect safety and identify possible neurological concerns. A crucial step in confirming the disorder is undergoing proper testing, especially when the condition may be progressive. To ensure accuracy, specialists rely on a REM diagnosis protocol that integrates:
- Detailed medical and neurological history
- Evaluation of nighttime behaviors
- Recording of dream-related physical actions
- Interviews with the patient and their bed partner
- Screening for medications or conditions that could trigger symptoms
However, the gold standard for identifying REM behavior disorder is a nighttime sleep study, particularly polysomnography for RBD, which monitors:
- Brain waves
- Eye movements
- Muscle activity
- Heart rate
- Breathing patterns
- Limb movements
This test allows clinicians to observe dream enactment behaviors in real time and distinguish them from other disorders.
Identifying Risks: Why RBD Should Never Be Ignored
Beyond nighttime restlessness or injury, REM behavior disorder carries broader long-term implications. Studies show that many individuals diagnosed with it may develop neurological conditions years or decades later. Monitoring and early intervention are crucial for long-term health management.
Risks associated with this disorder include:
- Repeated injury to self or partner
- Worsening sleep quality leading to chronic fatigue
- Heightened psychological stress
- Progression of underlying neurological issues
- Increased safety hazards in the bedroom environment
- Higher likelihood of coexisting sleep disorders
Understanding these risks helps patients and clinicians implement preventive and protective strategies early.
Treatment Strategies: How Sleep Clinics Manage RBD
While there is no single cure for REM behavior disorder, treatment focuses on improving safety, managing symptoms, and supporting long-term neurological health. Effective treatment plans may include:
- Medication adjustments to stabilize REM cycles
- Melatonin or targeted pharmacologic therapies
- Cognitive and behavioral sleep interventions
- Creating a safe sleep environment to minimize injury risk
- Monitoring of neurological changes over time
- Lifestyle habits that support better sleep regulation
- Avoiding alcohol or substances that worsen symptoms
At 8 Hours Sleep Clinic, treatment plans are customized for every patient, taking into account their overall health, nighttime behavior patterns, and long-term neurological profile.
Conclusion
REM sleep behavior disorder isn’t just a nighttime disturbance—it’s a significant neurological and sleep-related condition that requires early recognition and professional evaluation. Understanding the signs, taking note of risky behaviors, and seeking timely clinical support can make an enormous difference in both short-term safety and long-term health. With the right interventions and a specialized sleep care team, patients can regain secure, restorative sleep while safeguarding their well-being for the future.

